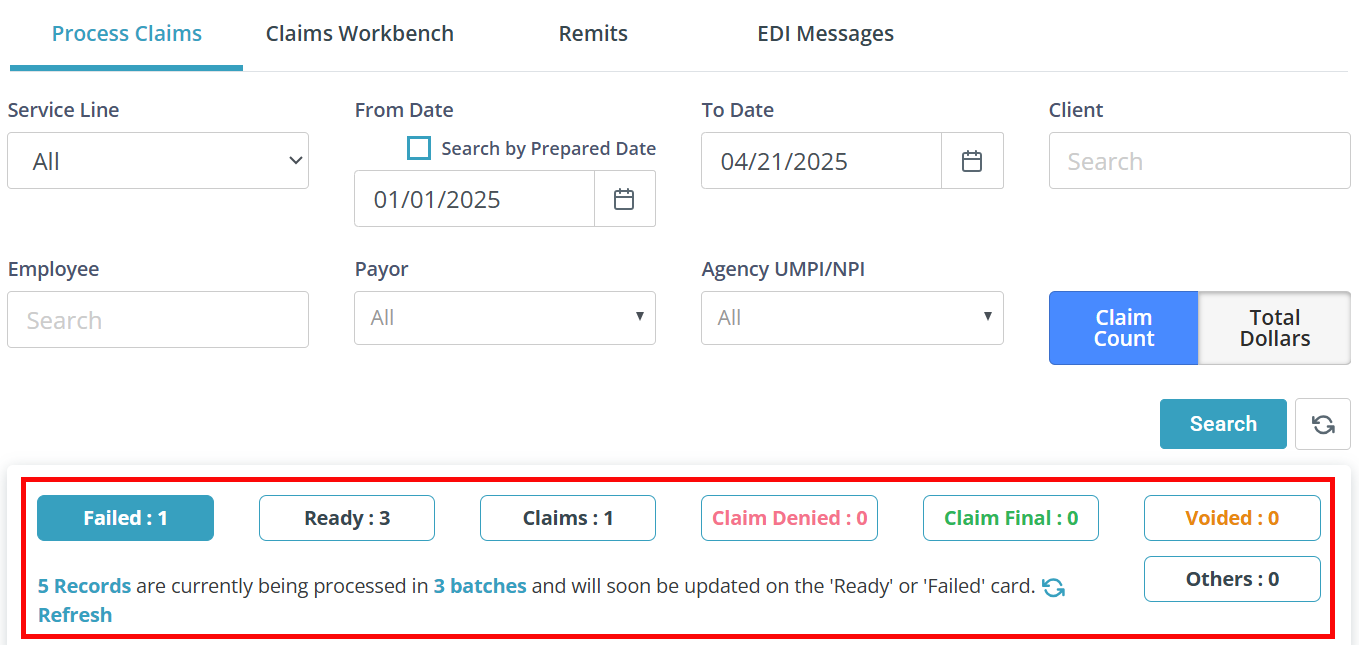
Claims Management Page
The Claims Management page is found under Financials > Claims Management and allows you to view the status and progress of claims throughout the billing process.
Start by selecting the Service Line, From Date, To Date, and then click the Search button. The data displays based on the dates that you have entered. You can only search 1 year at a time.
If applicable, enter the Client name and select a Payor. If searching for all claims, leave the Client search field blank and set Payor to All. Click the Search button.
Claims are divided into sections, or cards, depending on their status:
-
Failed: This card contains records that have issues and need your attention. Research the issue, make the necessary corrections, and re-validate them so you can submit successful claims. For more information on how to resolve failed claims, see Common Failed Claims and Resolutions.
-
Ready: This card allows you to identify and select records that are waiting to be sent to the Payor. It is important to review these records prior to sending them to the Payor.
-
Claims: Claims are records that have been sent to the Payor. Here you can keep an eye on the statuses of the claims, For MN DHS, Pavillio indicates where the specific claim is in the submission process: In Transit, Accepted, Will Pay, Will Deny, etc.
For MCOs you will see the Accepted status until the remit posts for most MCOs. MCOs do not send a 277 response file, so Pavillio can't display the other other status codes. Accepted indicates that Availity has accepted the claim for processing the Payor.
-
Claim Denied: Here you can select the claims you would like to find resolutions for and move them to the Claims Workbench where you can easily see and work through denied claims. It is a best practice to only move claims that you are working on at that time to the Claims Workbench, and not move all the claims at once.
-
Claim Final: Claims that are fully paid display here. If you need to rework claims that have been fully paid, select them and move them to the Claims Workbench.
-
Voided: Claims that have been voided in the Claims Workbench, sent to the payor, and confirmed as processed on the remit will display here.
-
Others: Records or claims that have been written off or marked as a spenddown display here.

When visit records enter Claims Management, they are automatically validated through a claim scrubbing process to identify issues that could result in denials. Many of these validations are compliance checks, such as confirming that a care delivery document exists on file for the client.
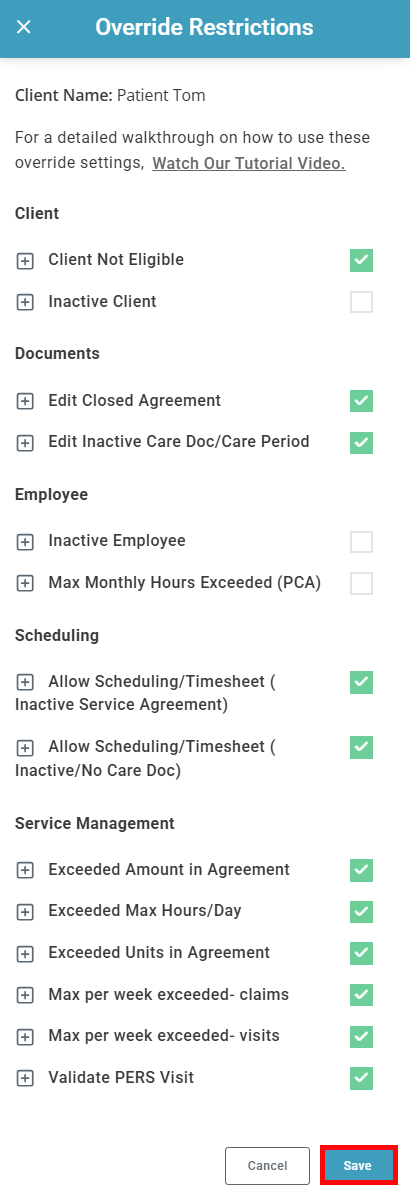
In certain scenarios, a biller may need to bypass specific validations in order to proceed with claim submission. The override function enables this by allowing the record to bypass designated restrictions while still moving forward in the workflow.
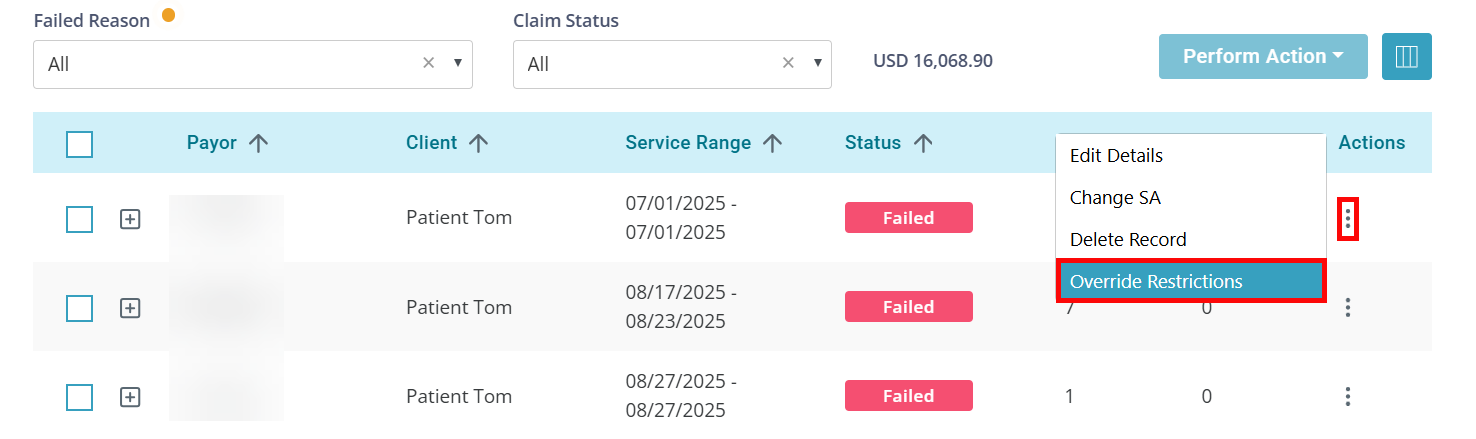
Overrides can be applied directly from the Failed and Ready cards in Claims Management: